Homeostasis
Responding to the environment
Organisms respond to their external environment to increase their chances of survival e.g. running away from a hungry lion. They also respond to their internal environment to ensure the conditions are optimal for metabolism (e.g. eating in response to hunger, or shivering when cold). A change in the internal or external environment is called a stimulus.
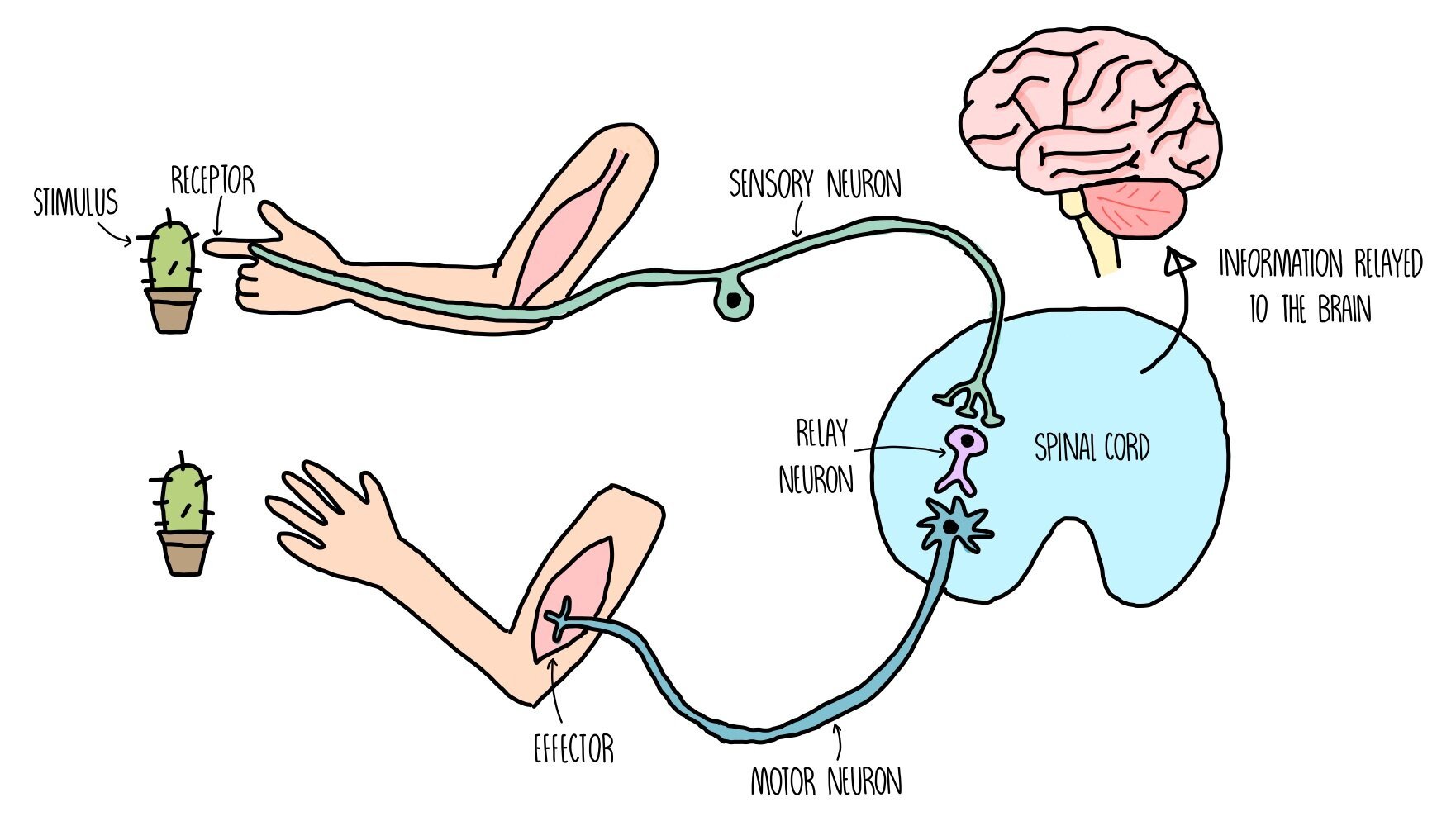
How the nervous system works
The nervous system detects changes in our environment (known as stimuli) through cells called receptors.
Receptors are sensitive to a number of different aspects of our environment, such as light, pressure (touch) and chemicals in the air (smell).
When receptors detect certain stimuli, they signal to the central nervous system (CNS) through initiating an electrical impulse through a neuron (nerve cell).
The neuron which sends an electrical impulse from the receptor within the sense organ and the coordination centre is called the sensory neuron.
The coordination centre receives impulses from various receptors around the body, processes the information and coordinates a response by signalling to other parts of the body. Coordination centres include the brain, spinal cord and pancreas.
These organs will signal to an effector (a muscle or gland) by releasing an electrical impulse along a motor neuron.
Relay neurons transmit impulses between sensory and motor neurons.
Stimulation of an effector will produce a response such as muscle contraction or hormonal release.
Cell signalling
Communication between receptors and effectors occurs by cell signalling, which can occur between adjacent or distant cells. For instance, neurons communicate by releasing chemicals called neurotransmitters which are detected by adjacent neurons, while cells in the pancreas communicate to distal cells by releasing hormones such as insulin, which travels around the body in the bloodstream. Chemicals like neurotransmitters and hormones are recognised by target cells using receptors on their cell surface membrane.
Homeostasis
Homeostasis is the maintenance of a constant internal environment. Things like our temperature, blood pH and blood glucose concentration needs to stay relatively stable in order to keep our cells functioning effectively. If internal conditions such as temperature or pH within our bodies don’t remain within certain limits, then enzymes will become denatured. Fluctuations in temperature result in hydrogen bonds breaking within the enzyme’s structure whereas changes in pH cause hydrogen and ionic bonds to break. The enzyme loses the shape of its active site and can no longer catalyse important biological reactions, such as respiration or DNA replication.
Negative and positive feedback mechanisms
Conditions within our bodies which are subject to homeostasis (such as temperature, pH and blood glucose concentration) are controlled by negative feedback mechanisms. These are mechanisms which act to reverse a change in the body - i.e. if temperature increases, a negative feedback mechanism ensures that changes to our body occurs in order to reduce our body temperature. The change in our body is detected by receptors (e.g. thermoreceptors which detect temperature or chemoreceptors which detect pH) and the reversal of the change is brought about by effectors (such as sweat glands which can modify the amount of sweat produced in order to change our body temperature). Negative feedback mechanisms therefore enable conditions within our body to remain within certain limits, fluctuating around the normal level.
In contrast, positive feedback mechanisms will amplify a detected change, moving conditions away from the normal level. They are used to accelerate a biological pathway, for example, the formation of a blood clot after an injury. At the site of a wound, activated platelets release a chemical which results in further platelet activation. This causes platelets to rapidly accumulate at the site of the wound, forming a blood clot. Positive feedback is not involved in homeostasis, because it does not keep internal conditions within a normal range.
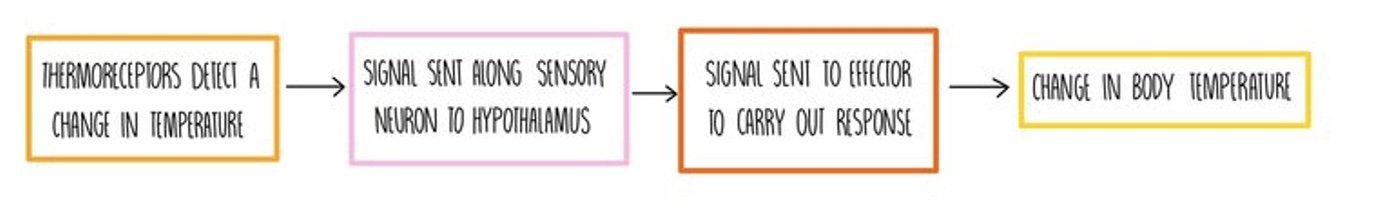
Control of body temperature
Any changes in our body temperature are detected by specialised receptors which are sensitive to temperature, called thermoreceptors. The thermoreceptors send a nerve impulse along a sensory neuron to a part of the brain called the hypothalamus, to indicate that a change in temperature has occurred. The hypothalamus sends a nerve impulse along a motor neuron to an effector. An effector is a muscle or a gland which can carry out the following responses to modify body temperature:
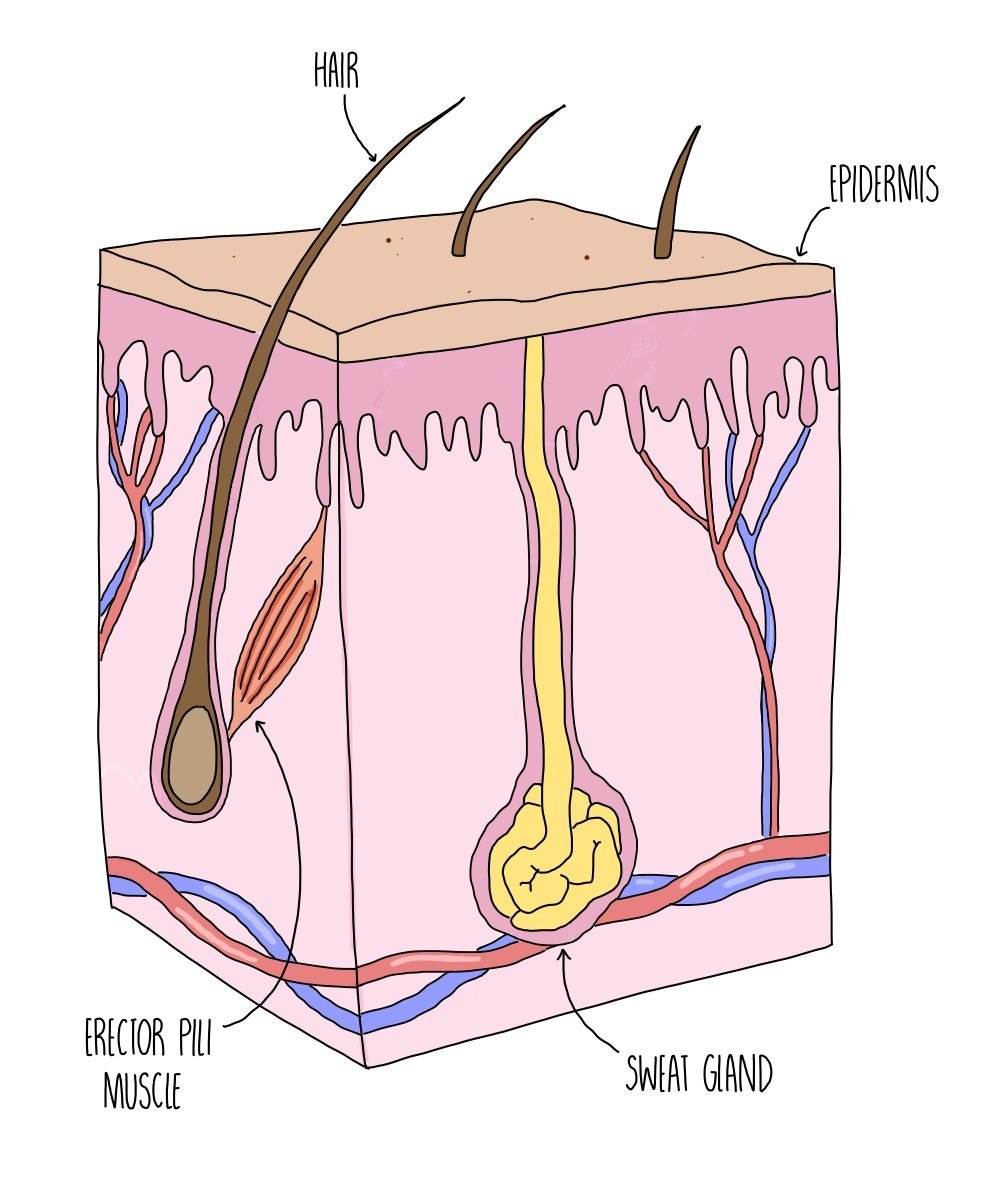
Responses to reduce body temperature:
Vasodilation - arterioles near the surface of our skin become wider (dilate), allowing more blood to flow through them. This increases the amount of heat that can be lost from the surface of our skin through radiation. This is the reason that you might look pink and flushed when you’re too hot.
Sweating - sweat glands increase the secretion of sweat. When sweat evaporates from our skin’s surface, it takes heat energy with it which cools us down.
Hairs lie flat - erector pili muscles underneath our skin relax, which causes the hair on our body to lie flat. Less air is trapped by the small hairs on our skin, making us feel cooler (since air is a good insulator).
Responses to increase body temperature:
Vasoconstriction - arterioles near the surface of our skin become narrower (constrict), so less blood is able to flow through them. This minimises the amount of heat that can radiate from the surface of our skin.
Reduced sweating - sweat glands reduce the secretion of sweat. Sweat normally cools us down by removing heat energy from our bodies when it evaporates, so the less sweat secreted, the less heat is lost.
Hairs stand up - erector pili muscles underneath our skin contract, which causes the hair on our body to stand on end. The hair traps a layer of air which is a good insulator, preventing heat loss from our body.
Shivering - muscles contract in spasms, increasing the amount of respiration inside the muscle. Heat is generated as a by-product of respiration.
Hormones - the hormones adrenaline and thyroxine are released. These hormones increase the amount of respiration happening in our bodies, resulting in the generation of more heat.
Control of blood glucose concentration
The concentration of glucose in the blood is one of the internal conditions that is kept constant with our bodies (homeostasis). It is monitored and controlled by the pancreas which releases a hormone called insulin if glucose levels become too high and another hormone called glucagon if levels fall too low. The action of insulin in reducing blood glucose levels and glucagon in increasing blood glucose are examples of negative feedback loops.
When blood glucose is high (i.e. after eating a meal):
Cells in the pancreas detect high blood glucose and stimulate beta cells in the islets of Langerhans to secrete insulin.
Insulin travels in the bloodstream to liver and muscle cells, where it binds to insulin receptors on their cell surface membrane.
Insulin increases the permeability of the membrane to glucose, so more glucose is moved from the bloodstream into cells. When insulin binds to its receptor, vesicles containing glucose transporters move and fuse with the plasma membrane.
It also stimulates the conversion of glucose into glycogen (glycogenesis) and an increase in the rate of respiration, which helps to lower blood glucose.
When blood glucose is low (i.e. running a marathon):
Cells in the pancreas detect low blood glucose and stimulate alpha cells in the islets of Langerhans to secrete glucagon.
Glucagon travels in the bloodstream to liver cells, where it binds to glucagon receptors on their cell surface membrane.
Glucagon stimulates the breakdown of glycogen into glucose (glycogenolysis) and a decrease in the rate of respiration, which helps to increase blood glucose.
It also triggers the production of glucose from non-carbohydrates, such as lipids and amino acids, in a process called gluconeogenesis.
Depolarisation of beta cells
Beta cells release insulin in response to membrane depolarisation:
High blood glucose causes increases glucose uptake into cells by facilitated diffusion.
Respiration rates increase, causing a rise in ATP.
Increased ATP causes potassium ion channels in the membrane to close.
Potassium ions are blocked from leaving the cell, so intracellular potassium ion levels rise.
The inside of the beta cell becomes less negative compared to the outside – the membrane is depolarised.
This triggers voltage-gated calcium ion channels to open and calcium ions move into the beta cell.
This stimulates the fusion of insulin-containing vesicles with the plasma membrane. Insulin is released by exocytosis.
Diabetes
Diabetes is a condition that results from the inability to control blood glucose levels. Uncontrolled blood glucose can be dangerous, so people with diabetes have to carefully regulate their carbohydrate intake and inject themselves with precise amounts of insulin. There are two types – type 1 and type 2 diabetes.
Type 1 diabetes
Onset in childhood – some cases appear to have a genetic component, others may be triggered by viral infection.
The immune system destroys the beta cells of the islets of Langerhans so that they can no longer produce insulin.
Results in sustained hyperglycaemia (high blood glucose) after a meal. Some glucose is excreted in the urine as the kidneys cannot reabsorb all of the glucose.
Treated with insulin injections or an insulin pump. The amount of injected insulin has to be carefully controlled to prevent glucose from dropping too low.
Patients also have to follow a carefully controlled diet.
Type 2 diabetes
Onset in adulthood – linked to lifestyle factors such as poor diet, obesity and lack of exercise. Also appears to have a genetic component as it is more common in those with a family history of diabetes.
Body cells stop responding properly to insulin because their insulin receptors stop working and their cells stop absorbing glucose, leading to elevated blood glucose levels.
Treated with a managed diet and regular exercise. In more severe cases, glucose-lowering drugs or insulin injections may be used.
Type 2 diabetes is becoming more common due to increasing availability of processed foods and low levels of physical exercise.
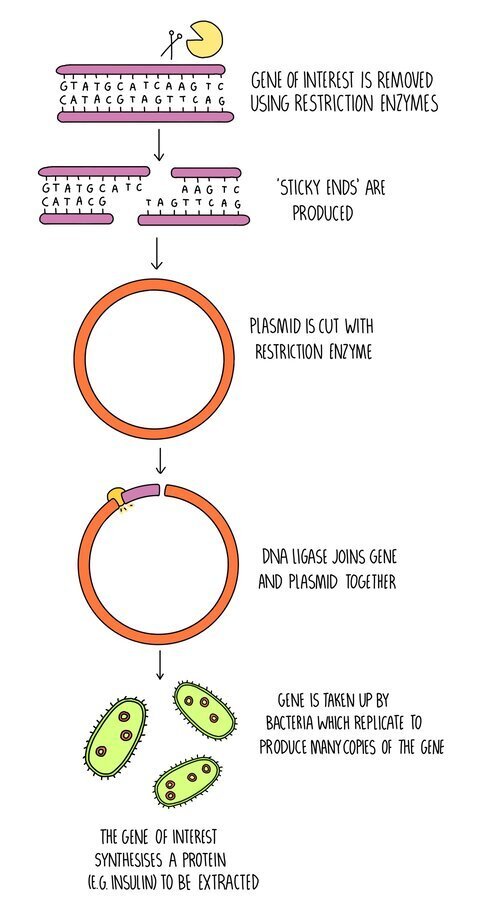
Producing insulin using genetically modified organisms (GMOs)
Genetically modified organisms (GMOs) are organisms which have had their DNA changed so that they synthesise proteins which can be used as drugs. Restriction enzymes are used to cut DNA at specific sites to extract a gene of interest. The same restriction enzymes are used to cut plasmid DNA, creating complementary sticky ends. DNA ligase joins the two pieces of DNA together so that the gene of interest is now contained within a plasmid. This is called recombinant DNA. This is either placed in a virus, which will infect organisms with the recombinant DNA, or the plasmid will be taken up by bacteria. Plasmids and viruses which carry the DNA molecule are called vectors.
This process is used for the production of insulin.
The insulin gene is removed from human DNA using restriction enzymes.
A plasmid is also cut with restriction enzymes.
DNA ligase joins the complementary sticky ends to form the recombinant DNA.
The recombinant plasmid is taken up by bacteria.
The transgenic bacteria are grown in large fermenters to produce large amounts of insulin, which can then be extracted.
Using stem cells to cure diabetes
Stem cells are undifferentiated (unspecialised) cells that can differentiate into any cell type. Scientists can use transcription factors to convert stem cells into pancreatic beta cells as a treatment for diabetes. The beta cells would be implanted into the pancreas of a person with type 1 diabetes, allowing them to synthesise insulin. The use of stem cells for diabetics is still being developed but may be used in the future as a cure for the disorder.