Immunity to Disease
Pathogens
A pathogen is any organism which causes disease. Infectious diseases (aka communicable diseases) are always caused by pathogens, which can spread from person to person to infect others. Non-infectious diseases (or non-communicable diseases), such as lung cancer or diabetes, are not caused by pathogens and tend to be more influenced by genetics or lifestyle factors.
Pathogens include bacteria, viruses, protoctists and fungi. Here are some examples of pathogenic organisms from each of these kingdoms:
Bacteria - Mycobacterium tuberculosis causes TB
Virus - HIV causes AIDS, COVID-19 causes coronavirus, the influenza virus causes seasonal flu
Protoctist - Plasmodium causes malaria
Fungi - Trichophyton causes Athlete’s foot
Communicable disease
Communicable diseases can be spread directly (e.g. droplet transmission of coronavirus through coughing or sneezing) or indirectly (e.g. the plasmodium parasite is spread through mosquito bites, transmitted between people that may never have met).
The transmission of a communicable disease is affected by the following factors:
Social factors – HIV may be underdiagnosed in countries with reduced healthcare access
Living conditions – overcrowding can increase the spread of diseases such as TB
Climate – tropical countries have ideal conditions for mosquitos to breed, increasing the prevalence of malaria
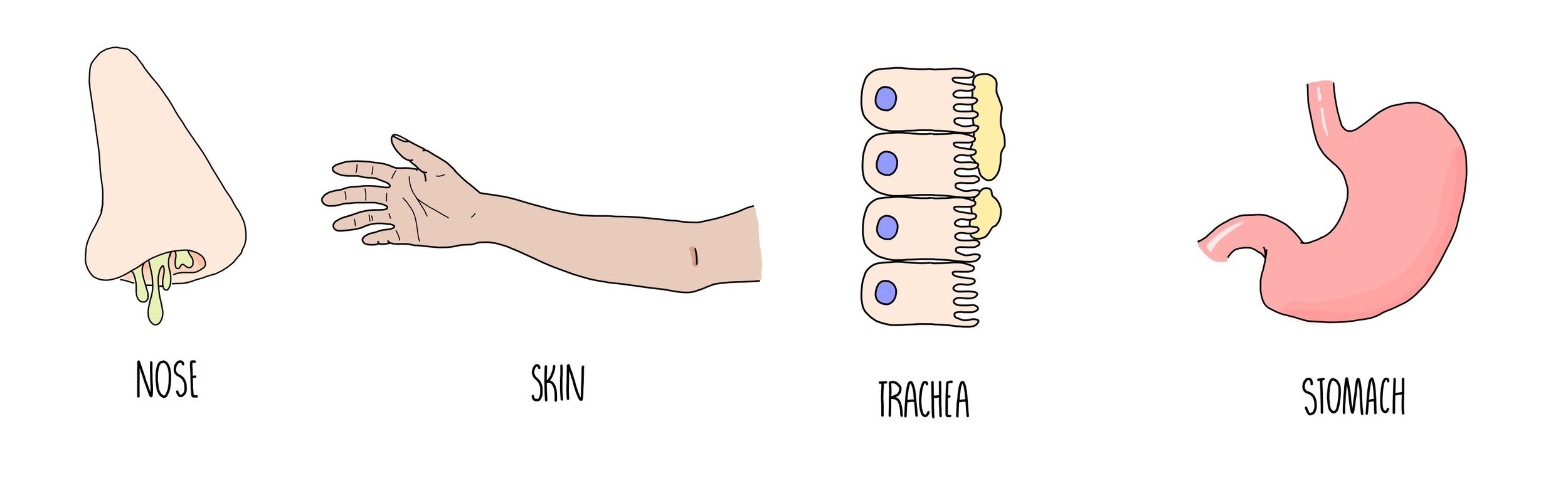
Barriers to prevent entry of pathogens
Our bodies have several defensive barriers to prevent us becoming infected by pathogens. For example:
Our body cavities (e.g. eyes, nose, mouth, genitals) are lined with mucus membranes which enzymes called lysozymes. Lysozymes kills bacteria by damaging their cell walls, causing them to burst open.
Our skin acts as a physical barrier to stop pathogens from getting inside of us. If our skin is cut or wounded, it is repaired by the outer layer of skin cells dividing and migrating to the edges of the wound. The tissue below the wound contracts to bring the edges of the wound together and fuse together by the formation of collagen fibres.
Blood clots form when blood vessels are damaged – this plugs wounds to prevent the entry of pathogens and blood loss.
The trachea (windpipe) contains goblet cells which secrete mucus. Pathogens that we inhale become trapped in the mucus, which is swept towards the stomach by the action of ciliated epithelial cells.
Our stomach contains gastric juices which are highly acidic - these will denature proteins and kill any pathogens that have been ingested in our food and drinks.
The insides of our intestines and the surface of our skin are covered in harmless bacteria which will compete with any pathogenic organisms and reduce their ability to grow.
When tissue damage occurs, it becomes inflamed. The swelling of inflamed tissue helps to isolate any pathogens that have entered the damaged tissue. Vasodilation increases blood flow to the area, helping white blood cells to arrive at the site of damage.
Expulsive reflexes such as coughing and sneezing help to expel pathogens from the body.
Plant defences
Physical defences:
The waxy cuticle on a leaf’s surface provides a physical barrier against the entry of pathogens into the leaf.
Any pathogens that make it past the cuticle then have to get past the cell wall, another physical barrier to pathogen entry.
When pathogens invade plants, they deposit a polysaccharide called callose between the cell wall and plasma membrane, making it harder for pathogens to enter cells.
Chemical defences:
Some plants produce antibiotic or fungicidal compounds – these kill or inhibit the growth of bacteria and fungi respectively.
Some plants produce insecticides (chemicals which are toxic to insects) – this reduces the risk of infection by plant viruses transmitted by insect vectors.
Antigens trigger an immune response
Pathogens possess molecules (usually proteins) on their cell surface called antigens which trigger an immune response when detected by our immune system. When an antigen is detected the immune response undergoes four main stages: phagocytosis of pathogen, activation of T lymphocytes, activation of B lymphocytes and production of antibodies by plasma cells.
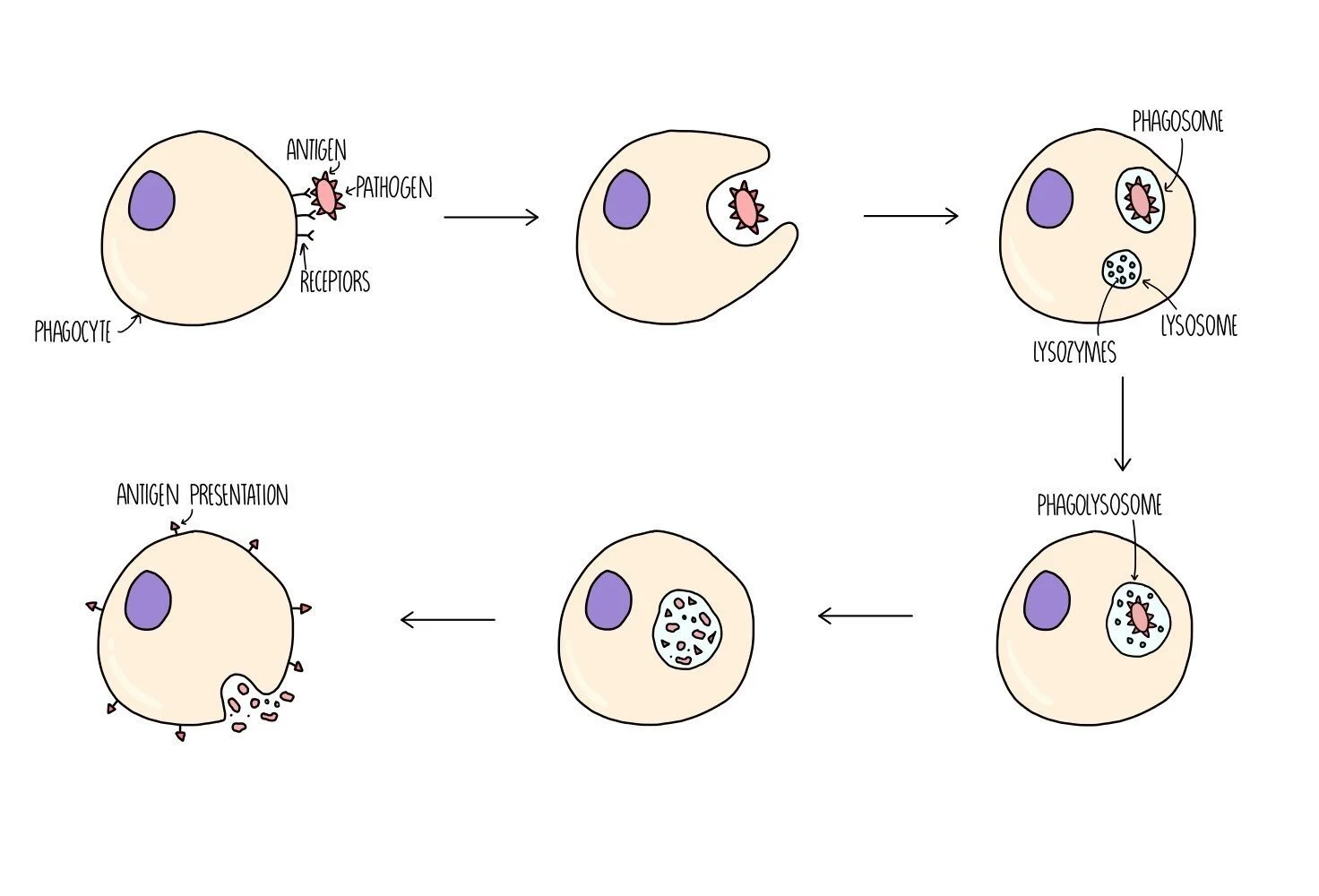
Phagocytosis
Phagocytes are a type of white blood cell which can destroy pathogens - types of phagocyte include macrophages, monocytes and neutrophils. They first detect the presence of the pathogen when receptors on its cell surface bind to antigens on the pathogen. The phagocyte then wraps its cytoplasm around the pathogen and engulfs it. The pathogen is contained within a type of vesicle called a phagosome. Another type of vesicle, called a lysosome, which contains digestive enzymes (lysozymes) will fuse with the phagosome to form a phagolysosome. Lysozymes digest the pathogen and destroy it. The digested pathogen will be removed from the phagocyte by exocytosis but they will keep some antigen molecules to present on the surface of their cells - this serves to alert other cells of the immune system to the presence of a foreign antigen. The phagocyte is now referred to as an antigen-presenting cell (APC).
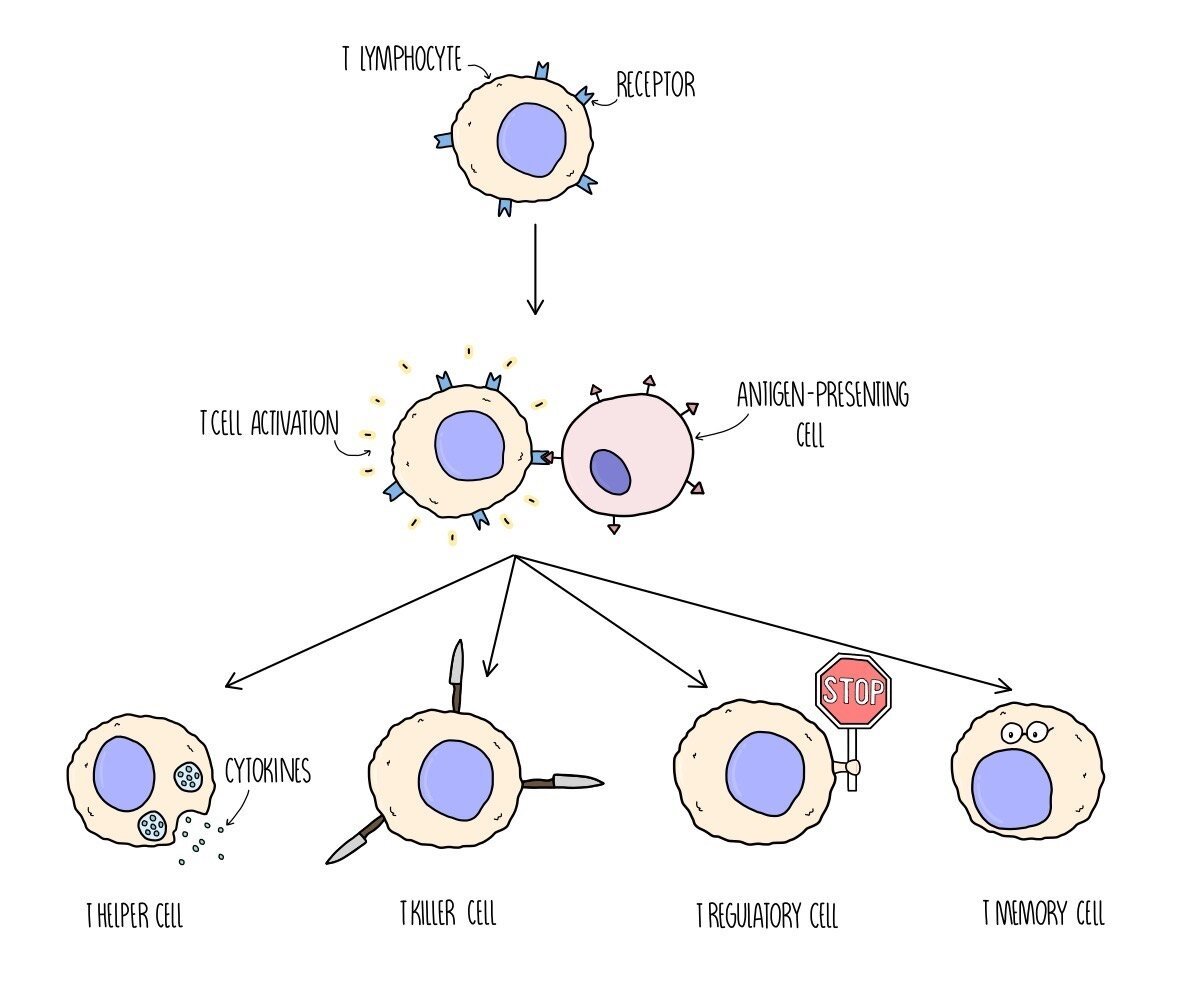
T lymphocyte response
T lymphocytes are white blood cells which contain receptors on their cell surface. Different T cells have different shaped receptors on their surface (so they will each bind to a different-shaped antigen). When a particular T cell binds to a complementary antigen (e.g. on a antigen-presenting cell or on a pathogen), the T cell will become activated - this is called clonal selection. Once it is activated, the T cell divides by mitosis to produce clones - this is called clonal expansion.
There are different types of T cell which play different roles in the immune response:
T helper cells release chemicals (they release a type of cytokine called interleukins) to activate B lymphocytes.
T killer cells (aka cytotoxic T cells) destroy any cells which have been infected with the pathogen.
T regulatory cells suppress other immune cells and prevent them from attacking our own (host) cells.
T memory cells remain in the bloodstream in low levels in case reinfection occurs. If the antigen is detected again at a later date, they will divide into T helper, T killer and T regulatory cells.
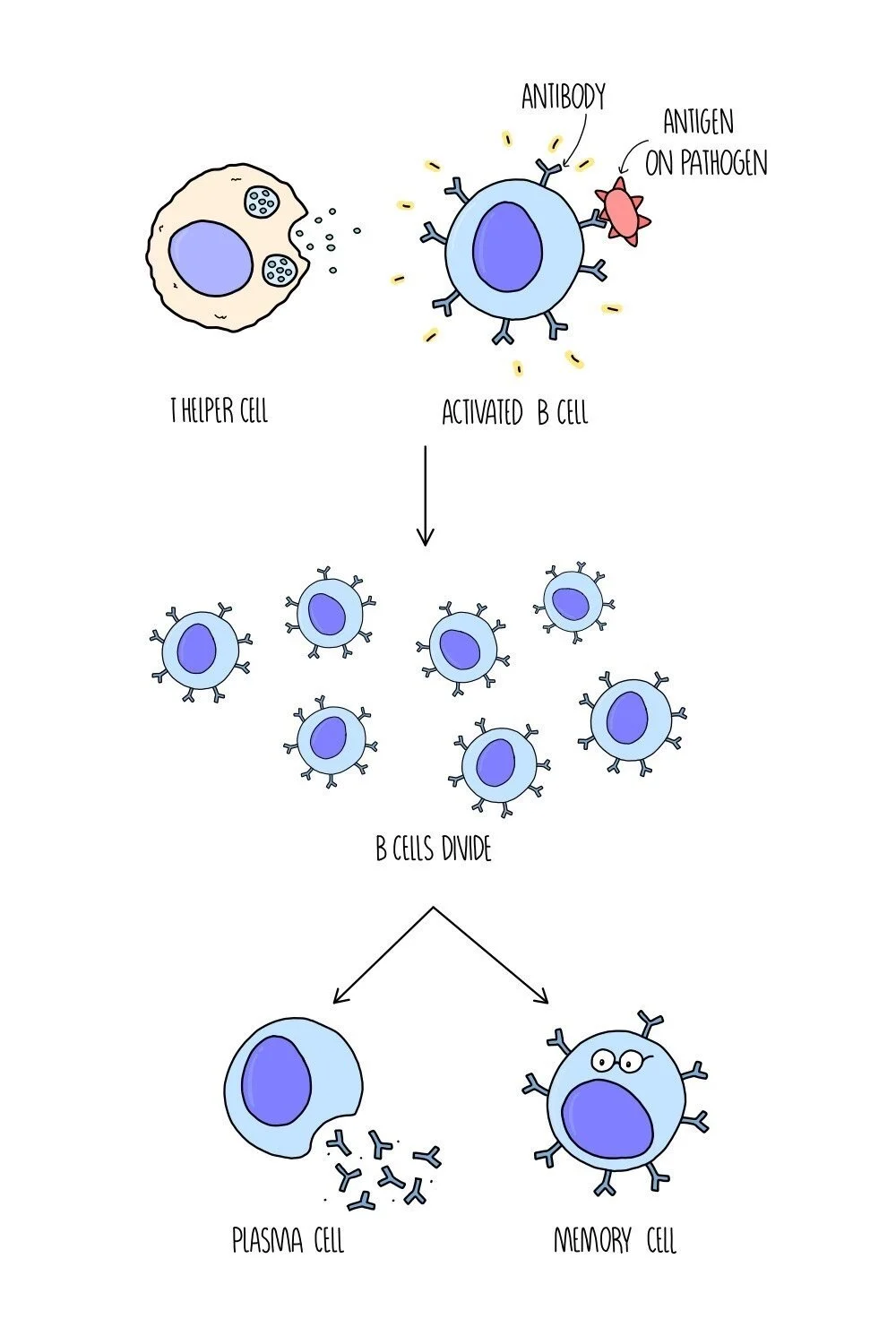
B lymphocyte response
B cells are activated when chemicals called cytokines are released from T helper cells. They are also activated when the antibody molecules on their cell surface bind to a complementary antigen. Different B cells have different shaped antibodies on their surface, so only the B cells with the correct-shaped antibodies will be activated.
Once they are activated, the B cells divide by mitosis and differentiate into two kinds of cell - plasma cells and memory cells.
Plasma cells produce antibodies with a complementary shape to the antigen.
Memory cells remain in the bloodstream in low levels in case reinfection occurs. If the antigen is detected again at a later date, they will quickly divide into plasma cells.
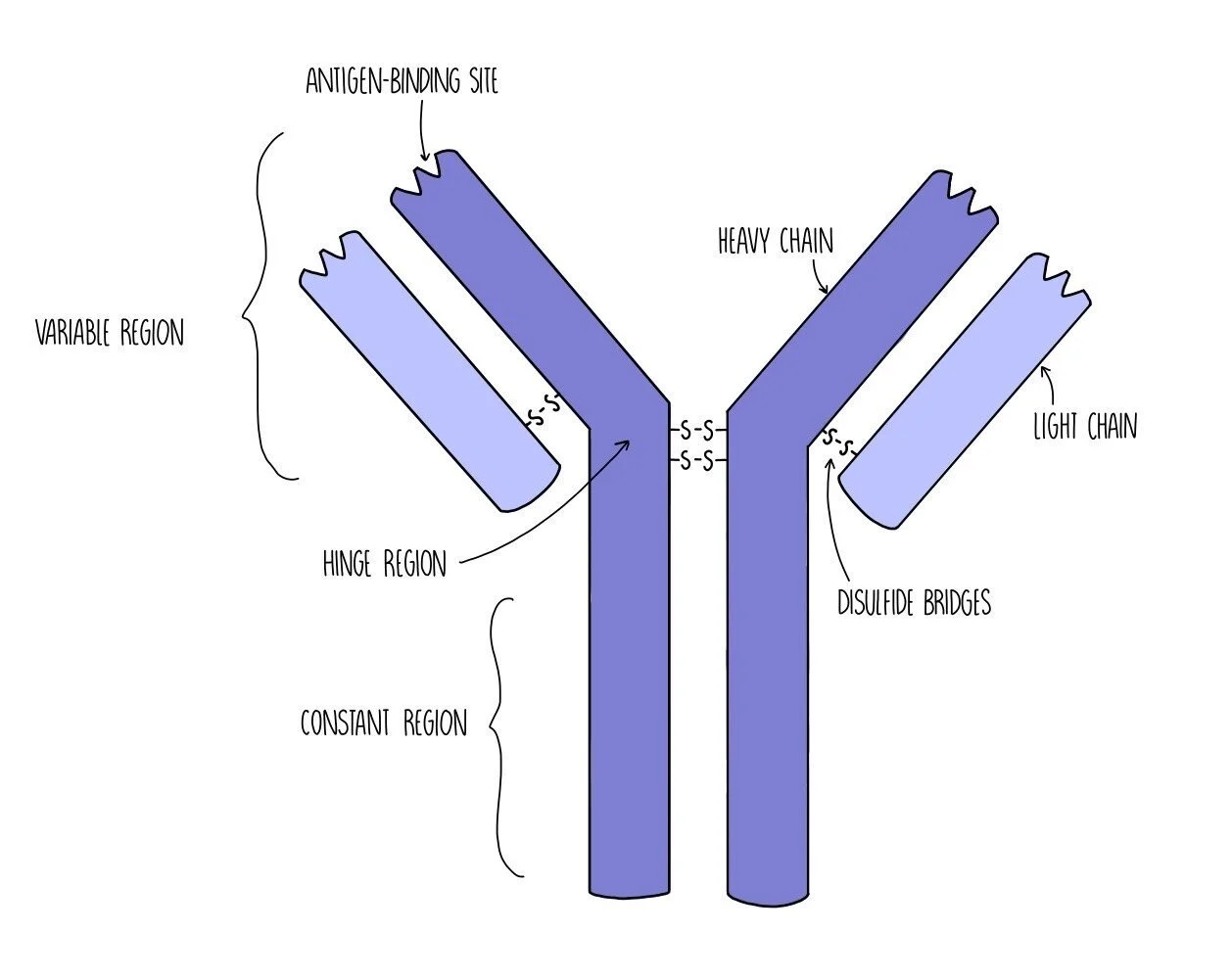
Antibody structure
Antibodies have a quaternary structure made up of four polypeptide chains (two heavy chains and two light chains) held together by disulfide bridges. They are composed of a variable region (which is different in different antibodies) where the antigen-binding site is located. The antigen-binding site has a complementary shape to the antigen which makes it specific to that particular antigen. There is also the constant region which is the same for all antibodies. The constant region contains another binding site which allows the antibody to bind to immune system cells, such as B cells or phagocytes. In between the variable region and the constant region is the hinge region which provides the antibody with flexibility.
How antibodies work
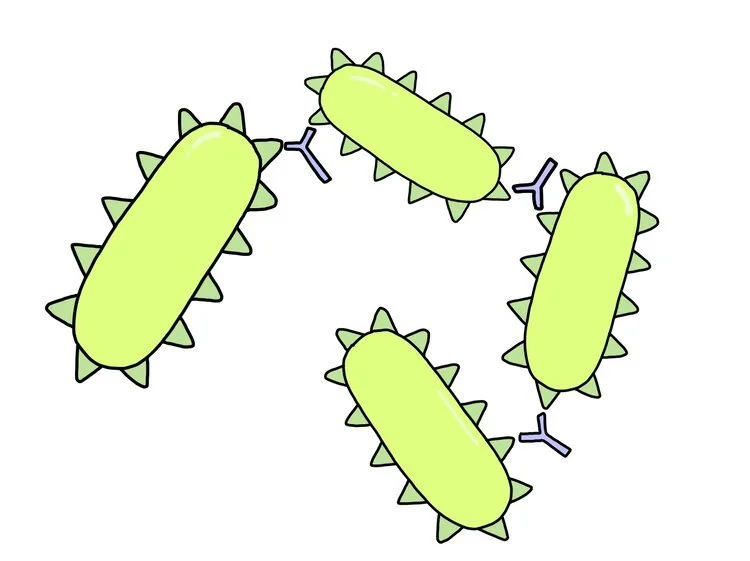
Antibodies work to destroy pathogens in three different ways.
Agglutination - antibodies each contain two antigen-binding sites which means they can bind to two pathogens at the same time. This causes pathogens to become clumped together. Phagocytes can then engulf and digest lots of pathogens at the same time, which makes phagocytosis more efficient.
Neutralising toxins - certain pathogens, such as bacteria, make us feel ill by releasing toxins. Antibodies can bind to toxins which renders them harmless (it neutralises them). The antibody-toxin complex can then be destroyed by phagocytes.
Blocking access to human cells - pathogens enter host cells when their antigens bind to receptor molecules on host cells (like a key opening a lock). When antibodies bind to antigens, it prevents the antigen from fitting in the receptor which means it can’t get inside the cell.
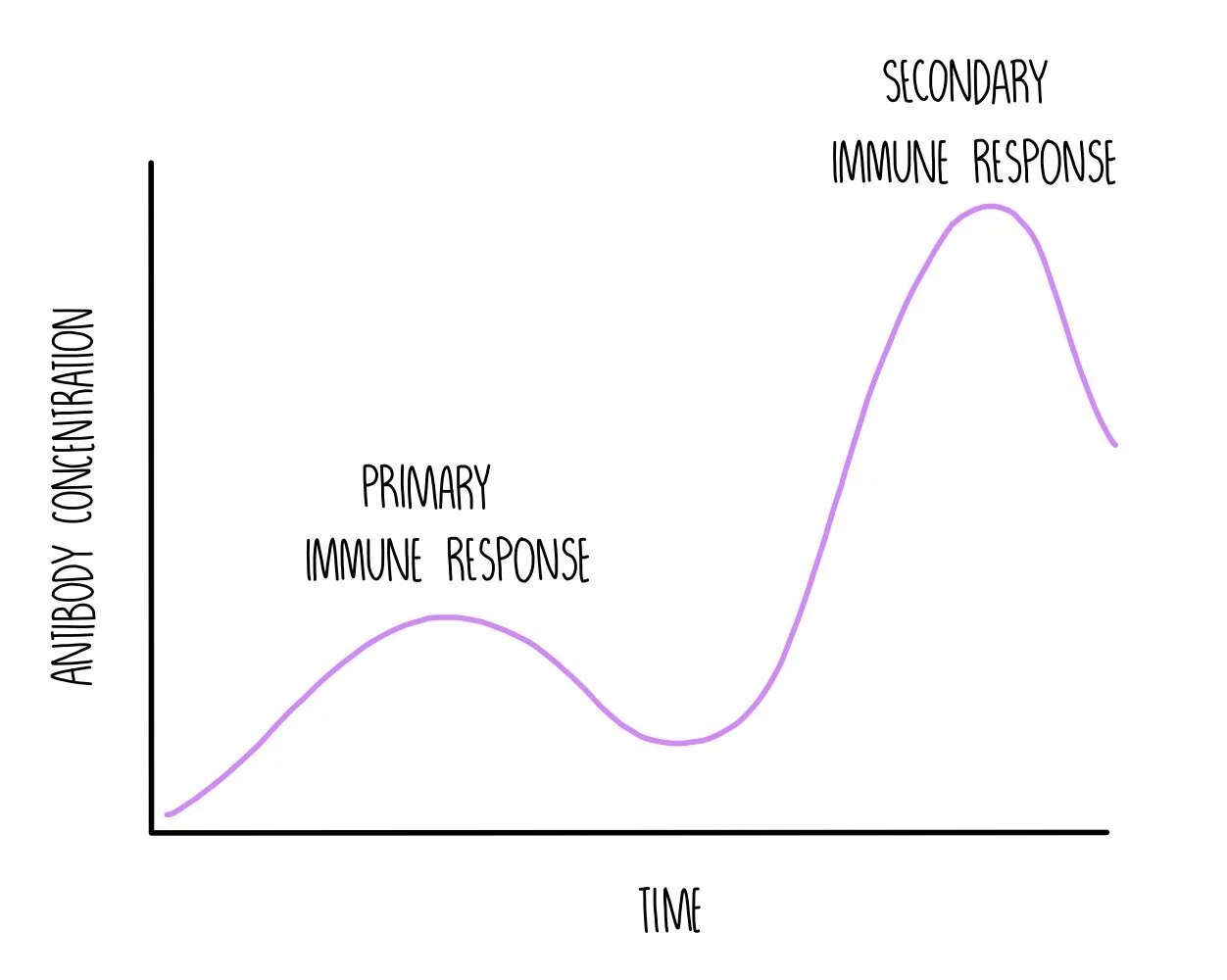
Primary and Secondary Immune Response
The primary immune response occurs when you are infected with a pathogen for the first time. It is composed of the non-specific and the specific immune response. This process is slow because it takes time for the correct B cell to be activated (clonal selection) and divide into lots of plasma cells (clonal expansion) in order to produce antibodies with a complementary shape to the antigen. The infected person will experience symptoms while the T and B cells mount an immune response. As part of the primary response, both T and B cells produce memory cells.
If you are re-infected with the same pathogen in the future, the T and B memory cells will recognise the antigen and start dividing. T memory cells will divide into the correct type of T killer cell to kill any cells that are infected with the pathogen. B memory cells will divide into plasma cells to produce a large number of antibodies which is complementary to the antigen molecules on the pathogen. This is the secondary immune response and is much quicker than the primary response. It happens so quickly that the pathogen is suppressed before you are able to experience symptoms - you are immune to the pathogen.
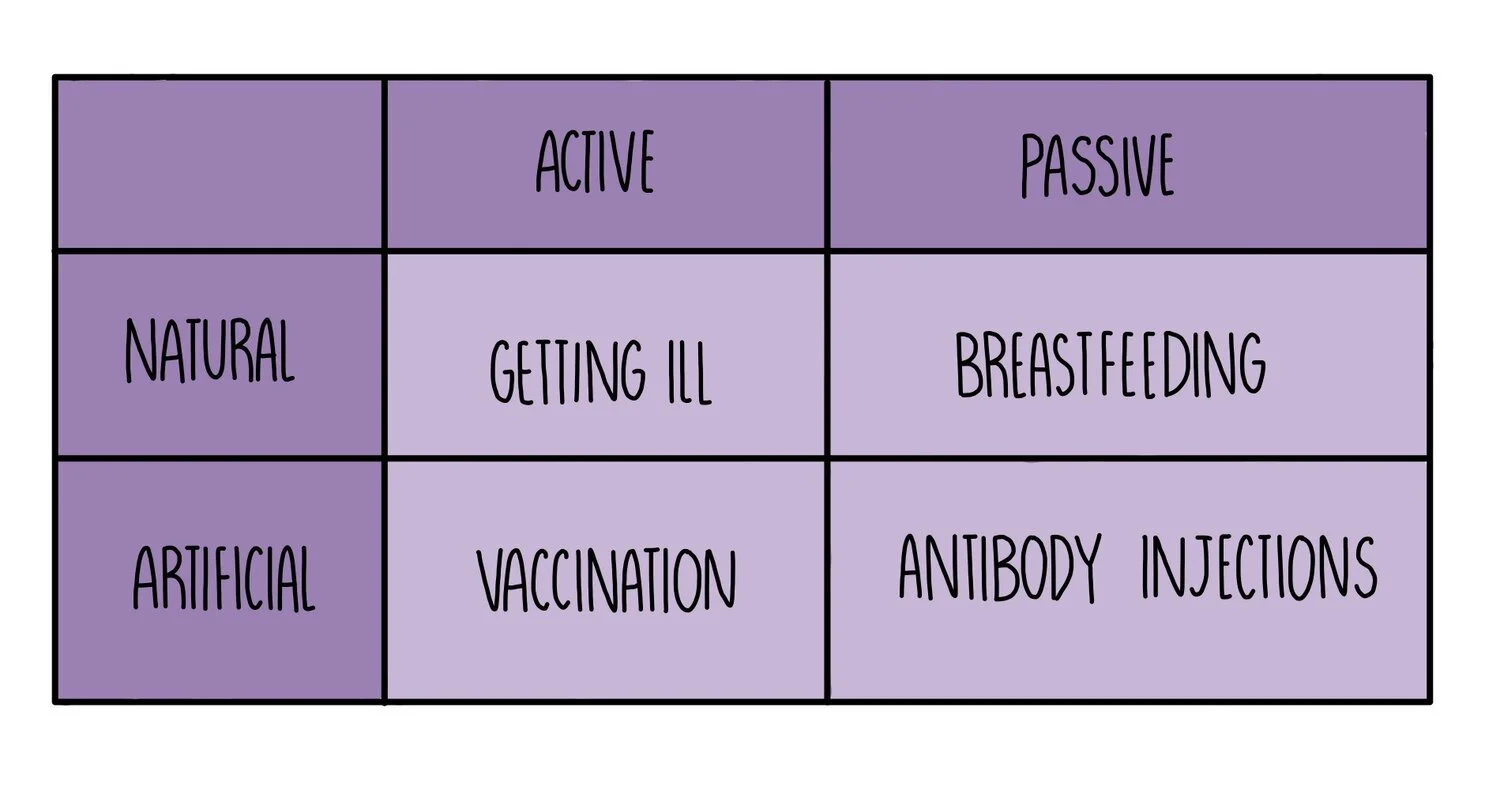
Active vs passive immunity
Active immunity occurs when your body makes its own antibodies after being stimulated by an antigen. This process can be natural (e.g. if you catch a cold, your body will make its own antibodies against the common cold virus) or it can be artificial (e.g. if you are vaccinated with a harmless form of an antigen).
Passive immunity occurs when you are given ready-made antibodies that have been produced by another organism. This process can be natural (e.g. babies receive antibodies from their mother when they breastfeed) or artificial (e.g. antibody injections can be given for some diseases - e.g. this is being tested as a treatment for Ebola).
Active immunity lasts longer since memory cells will remain in the body for years but it takes time to develop. Passive immunity provides immediate protection against pathogens but is short-lived (antibodies that are transferred from mother to child during breastfeeding only remain in the body for about 18 months).
Autoimmune disease
Autoimmune diseases occur when a person’s immune system fails to distinguish self-antigens from foreign antigens and starts attacking normal body cells. Rheumatoid arthritis is an autoimmune disease caused by the immune system attacking cells in the joints, leading to pain and inflammation. Autoimmune diseases are long-term (chronic) because there are currently no cures. However, patients can take medication to relieve their symptoms.
Vaccines
Vaccines contain a dead or weakened form of a pathogen which is injected into the bloodstream. Sometimes vaccines contain just the antigen proteins without the rest of the pathogen. Other vaccines might contain a variety of different antigens to protect against different strains of pathogens which vary in the shape of the proteins on their cell surface membranes (antigenic variation). The injection of weakened antigens stimulates a primary immune response and the production of memory T cells and memory B cells, resulting in immunity without becoming ill from the disease.
Antibiotics
Antibiotics work by interfering with bacterial cell walls and ribosomes, either killing the bacteria or stopping its growth. They have no effect on viruses or our own cells because:
Viruses do not have ribosomes or cell walls, which means that antibiotic treatment is completely ineffective against viral infections
Human cells do not have cell walls. We do have ribosomes, but these are bigger than those found in bacteria and unaffected by antibiotics. This is useful, because it means we can take antibiotics without worrying about it interfering with our own cells.
Antibiotic resistance
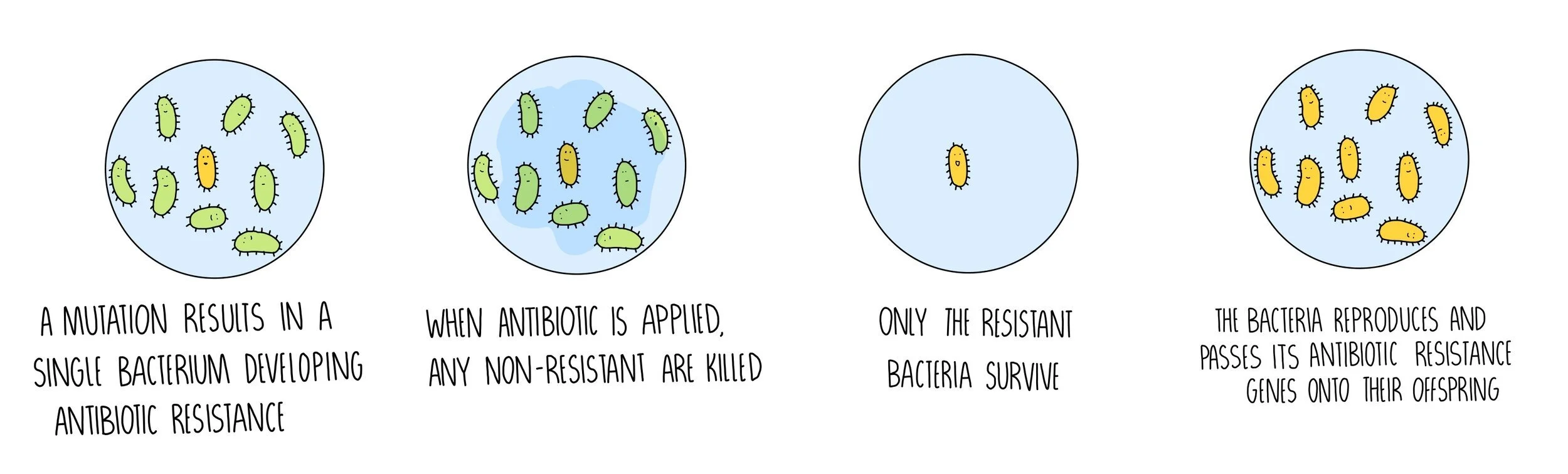
Bacteria can evolve quickly because they reproduce at a fast rate. Mutations in the bacteria’s DNA could make them resistant to certain antibiotics, such as penicillin, and will no longer be killed by the antibiotic. Evolution of the bacteria is an example of natural selection and supports Darwin’s theory of evolution.
A random mutation (DNA change) occurs in a single bacteria.
Some mutations protect the bacteria against the antibiotic.
These bacteria survive and divide to produce more bacteria containing the antibiotic-resistance gene.
Because antibiotic have been over-prescribed by doctors and due to their widespread use in farming, antibiotic resistance is becoming an increasing problem. MRSA is an example of a bacteria which has become resistant to most types of antibiotic. It is very difficult to treat and infections can be deadly. Clostridium difficile is another antibiotic-resistant bacteria that infects the digestive system. When antibiotics are used, all the non-resistant bacteria are killed, allowing C. difficile to grow unchecked. The bacteria secrete a toxin which causes diarrhoea and cramps.
Hospitals put measures in place to prevent the development of antibiotic resistance, including:
The rotated use of different antibiotics
Taking the full course of antibiotics
Avoiding overuse of antibiotics (e.g. for minor infections or for viral diseases).
Protecting sources of medicines
Many medicinal drugs originate from plants – for example, the antibiotic penicillin is secreted by a fungus. There are likely to be other useful antibiotics (and even drugs for targeting cancer or other diseases) synthesised in plants, fungi and bacteria that we are yet to discover. This means that it’s important to protect possible drug sources by maintaining biodiversity. Otherwise, some species may become extinct before their medicinal properties are discovered.
The future of medicine
Personalised medicine - people with different genetic profiles respond more effectively to some drugs than others. This means that doctors can use your DNA to tailor a treatment plan best suited to you.
Synthetic biology – technology is used to make artificial versions of cellular components or whole organisms already found in nature. It can be used for all sorts of things, including the manufacture of fragrances and improving the nutrient content of crops. It also plays an important role in the production of drugs.
Synthetic biology has been used to artificially produce the antimalarial drug artemisinin. The compound was first extracted from plants which were difficult to grow, limiting the availability of the drug and pushing up costs. Synthetic DNA is now used to produce the precursor to artemisinin which is inserted into yeast cells, which convert the precursor into the active drug.