The Liver and Kidneys
Excretion
Excretion is the removal of metabolic waste products from the body. For example, carbon dioxide is excreted when we breathe out and nitrogenous waste is excreted in the urine. These substances would cause tissue damage if allowed to accumulate, so excretion maintains homeostasis by keeping substances within a healthy range.
Liver function
The liver carries out multiple functions:
Breaks down amino acids into urea – this involves deamination followed by the ornithine cycle
Detoxifies the blood - alcohol, drugs and hormones in the blood are also broken down by the liver and their products are excreted from the body in the urine.
Stores glycogen – the liver converts excess glucose into glycogen.
Makes bile – bile aids lipid digestion by emulsifying fats.
The ornithine cycle
Excess amino acids can’t be stored and may damage tissues, so the liver converts them into urea in the ornithine cycle:
Amino acids are deaminated: the amino group is removed, forming ammonia and organic acids.
The organic acids are respired or stored as glycogen.
Ammonia is toxic so it is converted into a less harmful substance. Ammonia is combined with carbon dioxide, which converts it into urea in a cyclical reaction.
Urea is released into the bloodstream. It is filtered by the kidneys and excreted from the body in the urine.
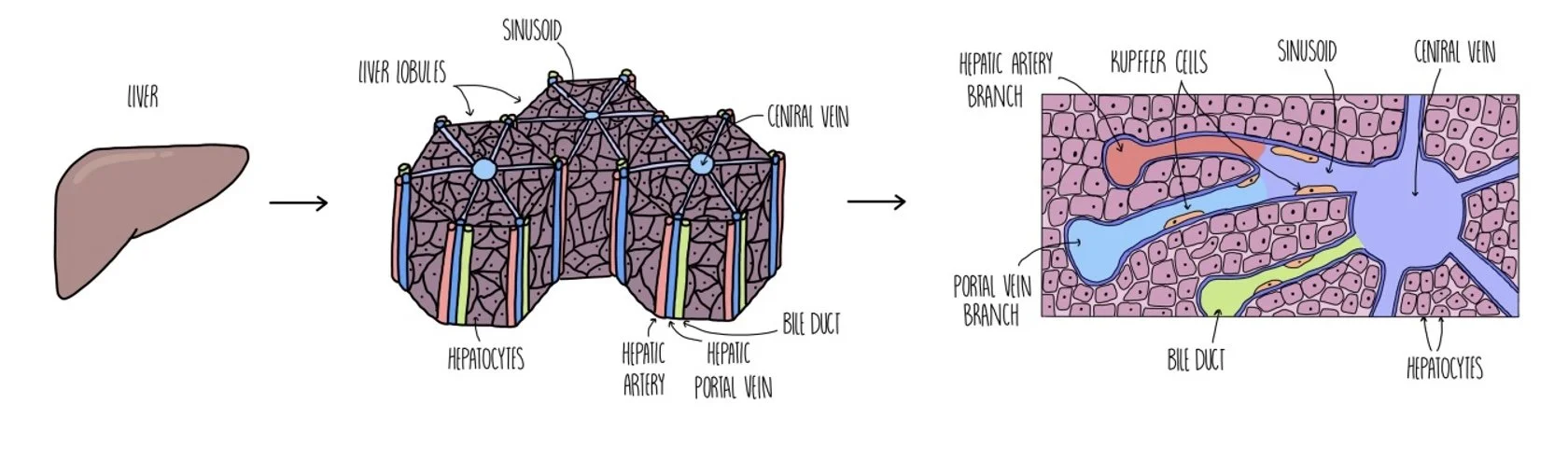
Liver structure
The liver contains the following vessels:
Hepatic artery – delivers oxygenated blood to the liver
Hepatic vein – takes deoxygenated blood away from the liver
Hepatic portal vein – connects the liver to the intestines. This allows harmful substances that have been removed from the liver to be immediately broken down.
Bile duct – takes bile from the liver to the gall bladder, where it is stored.
The liver is made up of liver lobules, which are cylindrical structures made up of hepatocytes (liver cells) that radiate out from the central vein. The central vein connects to the hepatic artery and hepatic portal vein via special capillaries called sinusoids. The central vein also connects to the bile duct via tubes called canaliculi.
As blood moves through the sinusoids, hepatocytes convert toxic substances into less harmful molecules. Kupffer cells that are attached to the walls of the sinusoids break down old red blood cells and remove bacteria from the bloodstream.
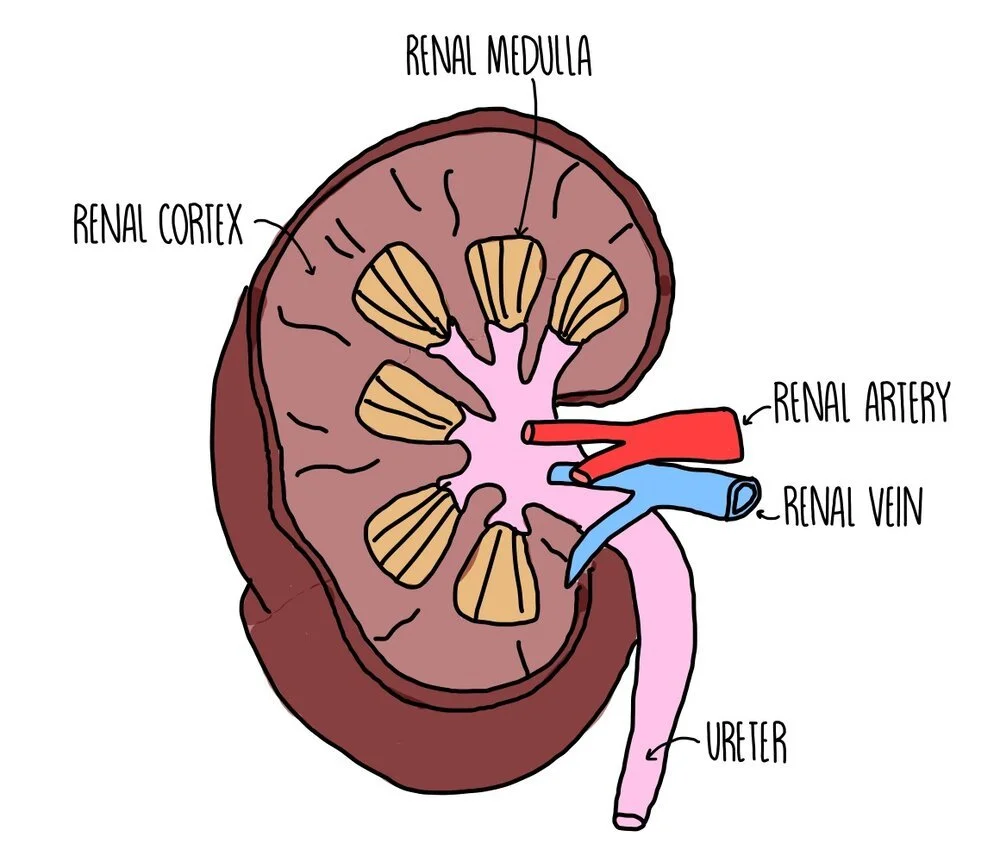
Kidneys
The inner part of the kidney is called the medulla and the outer part is the cortex. Blood is carried to the kidney via the renal artery for the kidney to filter the blood and remove waste products. The filtered blood is taken away from the kidneys by the renal vein. The individual structures which filter the blood are called nephrons.
Our kidneys remove excess water, excess ions and urea from our blood as urine. The removal of these substances from the bloodstream involves two processes: ultrafiltration and selective reabsorption.
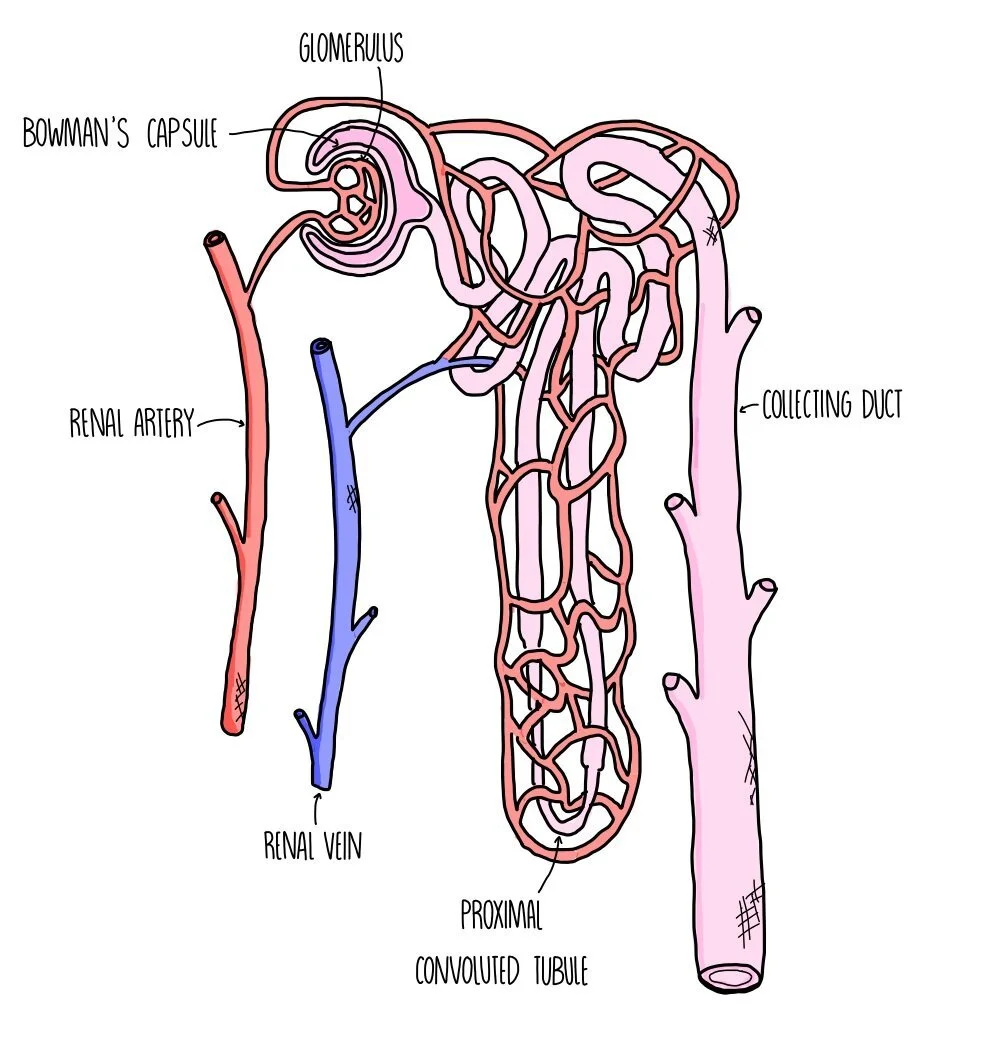
Ultrafiltration
The Bowman’s capsule surrounds a ball of capillaries called the glomerulus where blood is placed under high pressure. The efferent arteriole (leading away from the glomerulus) is smaller in diameter than the afferent arteriole (leading towards the glomerulus), so blood inside the glomerulus is under high pressure. Small molecules (glucose, urea, water and salts) are pushed out of the bloodstream and into the Bowman’s capsule, while larger molecules such as blood cells and protein stay inside the capillaries. They form a substance called glomerular filtrate, which moves through the nephron.
When small molecules pass between the capillary and the kidney, they pass through three layers: the capillary endothelium, the basement membrane and the epithelium of the Bowman’s capsule.
Selective reabsorption
In the proximal convoluted tubule (PCT), loop of Henle and the distal convoluted tubule (DCT), useful substances are reabsorbed, passing out of the nephron and back into the capillaries. Glucose is reabsorbed in the PCT by active transport and facilitated diffusion. The PCT epithelium has microvilli to provide a large surface area for reabsorption. Water is reabsorbed in the loop of Henle, DCT and collecting duct by osmosis. The remaining filtrate is urine, containing excess water, excess salts and urea. This passes from the collecting duct to the bladder via the ureter. Urine may contain additional substances like hormones, excess vitamins, the breakdown products of medications and recreational drugs.
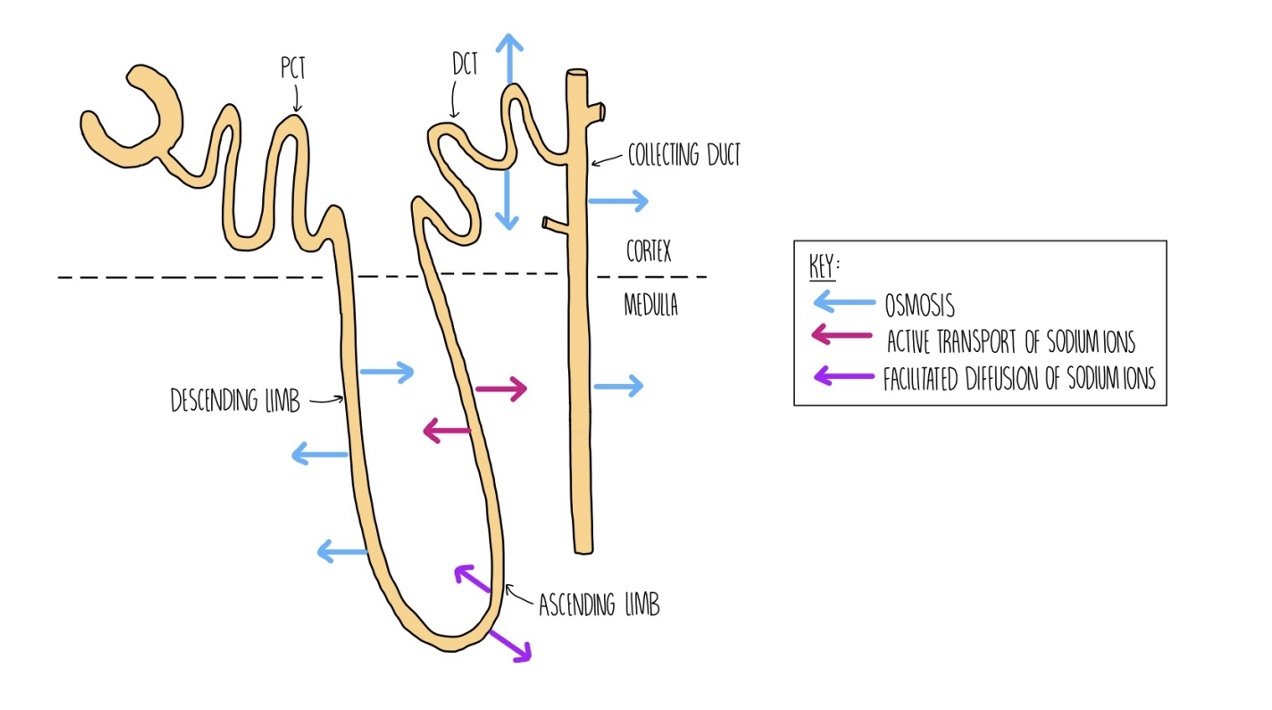
Water reabsorption
Water is reabsorbed along almost the entirety of the nephron, but regulation of water potential mostly takes place in the DCT, loop of Henle and collecting duct with the amounts of water reabsorbed controlled by hormones such as ADH.
The nephron spans two parts of the kidney – the Bowman’s capsule, PCT and DCT are in the cortex of the kidney while the loop of Henle and lower half of the collecting duct are located in the medulla. The loop of Henle is made up of two limbs called the ascending and descending limb, which control the movement of ions and allow water to be reabsorbed:
The ascending limb is permeable to ions but impermeable to water. At the top of the ascending limb, sodium ions are actively pumped into the medulla.
This lowers the water potential of the medulla, causing water to move out of the nephron by osmosis from the descending limb (which is permeable to water but not ions).
As water moves out of the nephron, the filtrate becomes more concentrated. This causes sodium ions to move out of the nephron at the start of the ascending limb, down their concentration gradient by facilitated diffusion.
This lowers the water potential of the medulla even further, causing water to move out of the DCT and collecting duct by osmosis.
Water that has moved into the medulla eventually moves into the capillary.
Organisms that live in dry conditions (e.g. camels) are adapted by having an extra-long loop of Henle. This means that more ions can be pumped into the medulla, encouraging more water to move out of the nephron by osmosis.
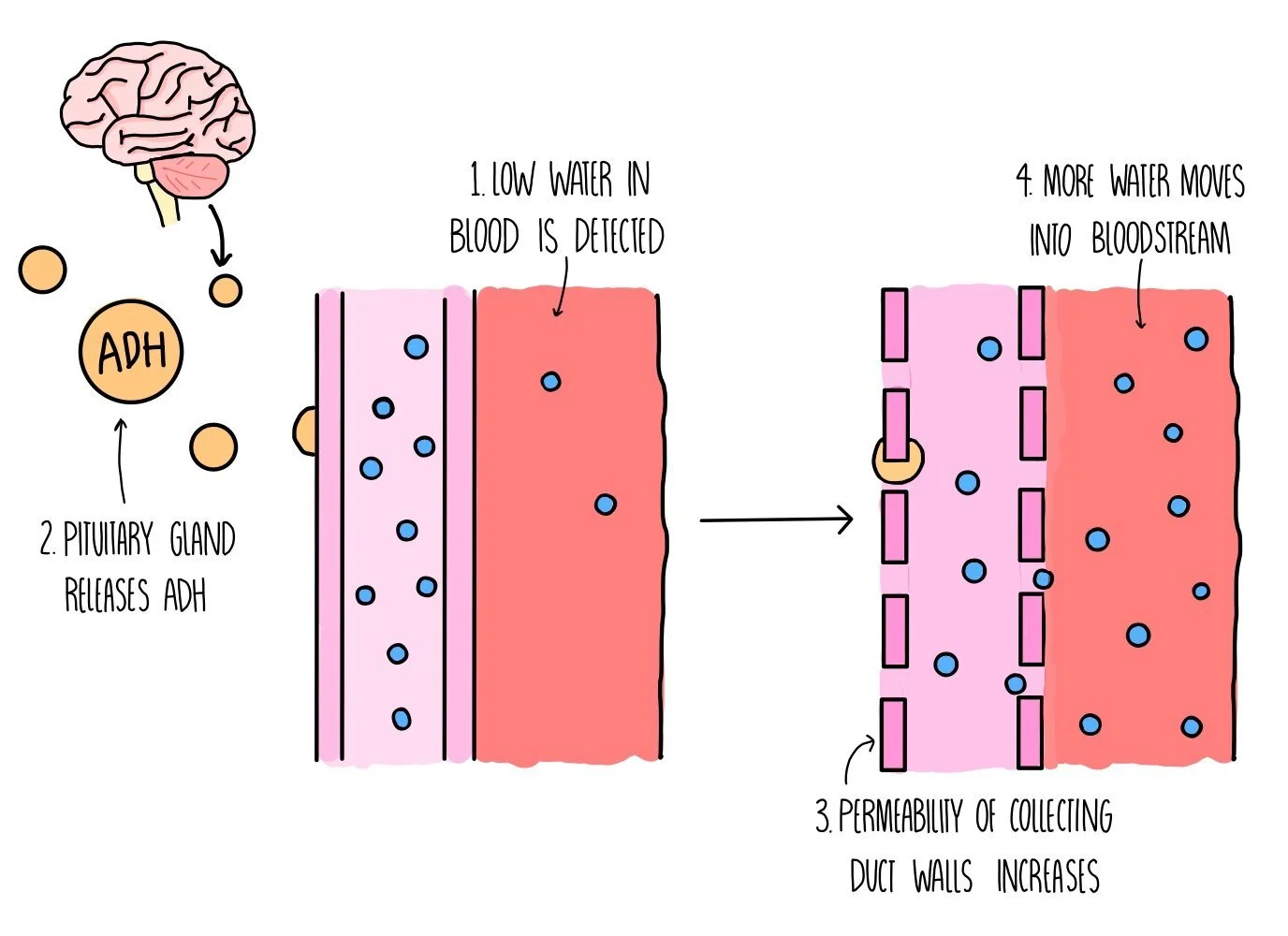
Antidiuretic hormone (ADH)
ADH controls the water content of our urine by increasing the reabsorption of water from the collecting duct. It works by increasing the permeability of the collecting duct wall, making it more porous and allowing more water to pass from the kidney into the bloodstream. It is released by the pituitary gland in the brain when water levels in our blood plasma are becoming low. This type of control is an example of a negative feedback mechanism:
Osmoreceptors in the hypothalamus detect a drop in blood water potential.
The hypothalamus signals to the posterior pituitary gland to secrete ADH.
ADH causes the walls of the DCT and collecting duct to become more permeable to water (by the incorporation of more aquaporins into the membranes of the cells that line these parts of the nephron).
More water moves by osmosis out of the DCT/collecting duct and reabsorbed into the bloodstream, increasing its water potential.
A smaller volume of concentrated urine is produced.
Kidney failure
Kidney failure occurs when the kidneys stop filtering toxic substances out of the blood. It can be caused by infection or high blood pressure. Infection leads to inflammation in the kidneys which damages cells, so the nephron cannot reabsorb substances properly. High blood pressure damages the glomeruli so that large molecules like proteins pass into the nephron and into the urine. It is diagnosed by measuring the glomerular filtration rate (GFR), the rate at which blood is filtered from the Bowman’s capsule. Low GFR indicates kidney failure.
Kidney failure can cause the following problems:
Build-up of waste products such as urea in the blood. Excess blood urea leads to vomiting and weight loss.
Ion imbalance – this can lead to acidic blood, brittle bones and water retention.
Accumulation of fluids in tissues – causes swelling of body parts
Anaemia – low blood haemoglobin
Mortality – kidney failure can lead to death if not properly treated.
Treating kidney failure
Illustration of a diseased kidney. Credit: Scientific Animations (Wikipedia)
Kidney failure can be treated with dialysis, which involves connecting the patient’s blood supply to a dialysis machine. Their blood is passed through a partially permeable membrane surrounded by dialysis fluid. The urea diffuses out of the blood and into the dialysis fluid, whereas glucose, water and salts move between the blood and dialysis fluid to reach normal concentrations. Dialysis involves multiple hospital visits where the patient is connected to the machine for long periods of time. In addition, the treatment is expensive and the patient still needs to maintain a carefully controlled diet.
Another form of treatment is a kidney transplant, however this requires major surgery and the associated risks. The new kidney may be rejected by the patient’s body so they are given immunosuppressant drugs which suppress the immune system and make the individual susceptible to other diseases. On the plus-side, it’s cheaper than regular dialysis sessions and provides the patient with a better quality of life.
Urine testing
Because substances that are removed from the blood end up in urine, it can be tested for the presence of drugs or compounds associated with disease/pregnancy.
Pregnancy tests – these detect the hormone human chorionic gonadotropin (hCG) that is found only in the urine of pregnant people. Pregnancy sticks contain monoclonal antibodies that are complementary to hCG and a bound to a coloured bead. If hCG is present, it binds to the antibodies. The urine moves up to the test strip, carrying the bound beads with it. Immobilised antibodies are fixed to the surface of the test strip, which will bind to any hCG on the hormone-antibody-bead complex. This causes the blue beads to become concentrated in the test area, turning the test strip blue. If the urine contains no hCG, nothing will stick to the immobilised antibodies and the test strip stays white.
Drug testing – the presence of drugs in urine can be detected using test strips which contain antibodies that the drug will bind to. If a certain amount of the drug is present, the test strip changes colour. This is usually followed up by further testing by gas chromatography/mass spectrometry (GC/MS). The technique involves vaporising the sample and passing it through a column containing a polymer. Different substances move through the column at different speeds, causing the substances in the urine sample to separate out. The separated substances are ionised in the mass spectrometer and identified based on their mass.
Testing for steroids – anabolic steroids are drugs that increase muscle mass. They are banned in competitive sports but some athletes may choose to take them, despite the dangerous side effects.